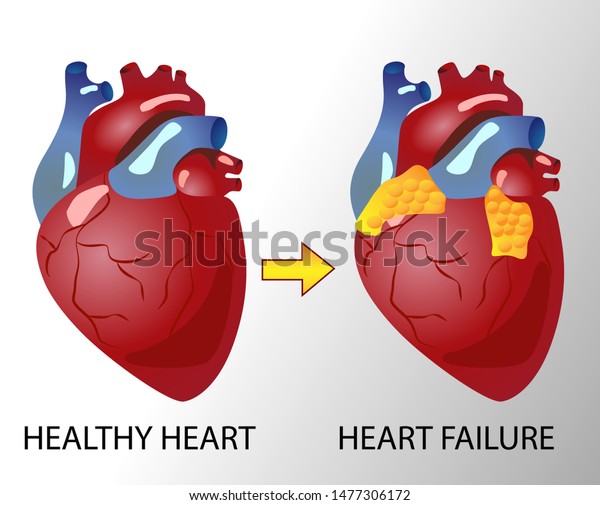
Heart failure is a chronic disease of the heart in which the heart can not pump enough blood according to the requirements of body tissues. When the supply and demand of oxygen are not in a balance because of low cardiac output, the condition is known as heart failure. The most common causes of heart failure are coronary artery disease, hypertension, arteriosclerosis, myocardial infarction, hypertension, cardiomyopathy, and congenital heart problem.
What is the physiology of a normal heart?
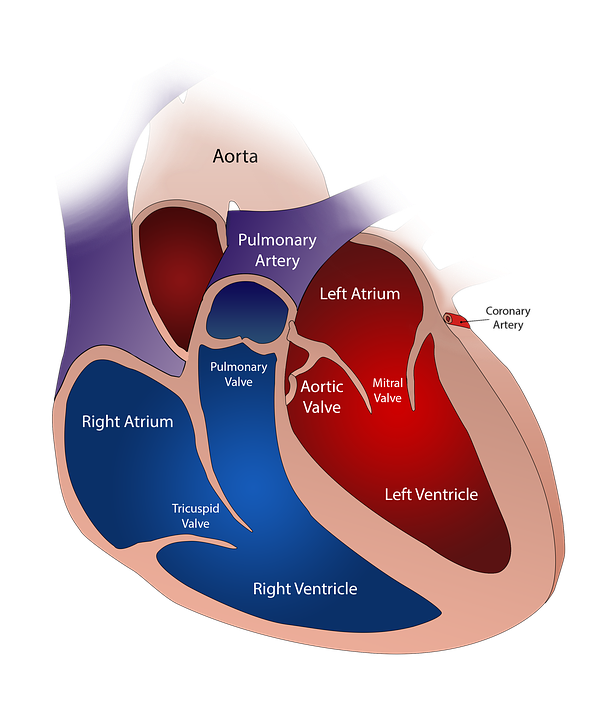
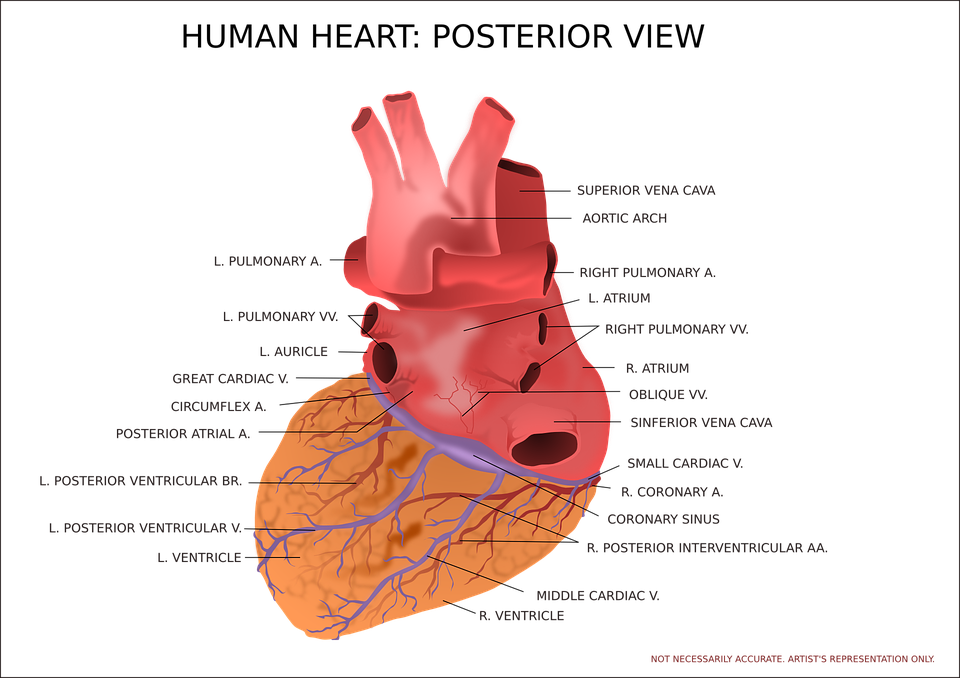
A normal heart is a strong muscular ■■■■■ within the pericardial sac (double-walled sac) having the size of a fist and located in the upper left quadrant of the human body. Physiology of heart can be explained by the process that, blood that is pumped by the heart, carries oxygen and essential nutrient to every cell of the body including the heart itself.
The heart consists of four chambers, with two upper and two lower chambers on each side. Upper chambers are known as atria (singular atrium) and the lower chambers are known as ventricles.
The process by which blood is supplied can be explained by the following steps:
- Blood from all over the body (de-oxygenated blood) is collected in the right atrium by veins.
- From the right atrium, this deoxygenated blood is sent to the right ventricle via the valves.
- Right ventricle contracts and blood is pumped towards the lungs for its oxygenation.
- Oxygenated blood from the lungs returns to the left atrium from where it is passed to the left ventricle.
- Left ventricle then contracts forcefully to supply the oxygen-rich blood to the whole body including the heart.
These chambers do not contract randomly, instead, they contract and relax in a highly organized sequence.
Summary
Heart consists of four chambers, two atria, and two ventricles. These chambers contract and relaxed in an organized manner to supply the blood and oxygen to every tissue of the body.
What are the types of heart failure?
There are two types of heart failure
- Systolic heart failure
- Diastolic heart failure
- Systolic heart failure is more common in young people. In systolic failure, there is a reduction in the force of contraction along with low ejection fraction.
- In diastolic heart failure, heart chambers are not filled properly because of hardening and inadequate relaxation, hence the output of the heart is decreased.
- When oxygen supply does not meet the oxygen demand, then the cells and tissues of the body try to keep the already present blood inside them, for the sake of supply to the brain and heart.
- This results in building up of fluid (edema) causing swelling in certain body areas for example ankles and feet.
Summary
There are two types of heart failure, systolic heart failure, and diastolic heart failure. When oxygen supply and demand are not in equilibrium, it results in heart failure.
What are the stages of heart failure?
There are four stages of heart failure named A, B, C, and D. Patient once moved to stage B can’t move back to stage A. Hence heart failure is a progressive disease.
1. Stage A
- This is the state of Pre-heart failure, which means that patient is at risk to develop heart failure. There are no structural heart disease or symptoms of heart failure.
- Patients may have a family history of heart disease and some comorbidities that may lead to heart failure.
Risk factors of heart failure in stage A are Hypertension, diabetes, obesity, metabolic disease, excessive use of alcohol, family history of cardiac disease, coronary artery disease, or use of medications that may cause heart failure
Treatment plan
Following the treatment plan is recommended to prevent further progression of heart failure.
• Adopting a healthy lifestyle involving exercise, regular walk, and maintaining body weight.
• Maintaining blood pressure by medication therapy and supportive treatment including low salt food.
• Taking Angiotensin-converting enzyme inhibitors, angiotensin receptor blockers or beta-blockers, in case of vascular disease, hypertension, or diabetes.
• Statins can also be an option.
2. Stage B
It is also a pre-heart failure stage but with structural heart disease. If a patient has been diagnosed with left ventricular dysfunction yet not having any symptoms of heart failure, it is considered that patient is standing at Stage B.
In this stage, the patient is having an ejection fraction of less than 40%, according to Echocardiogram (ultrasound of the heart).
Treatment plan
• All the factors mentioned in stage A treatment plan
• Beta blockers are especially used if the patient has had a heart attack (if not taking in stage A)
• Additionally, spironolactone (Aldosterone antagonist) is recommended to prevent heart enlargement (Cardiomegaly) if the patients have had a heart attack along with diabetes.
• Cardiac surgery may be an option in case of a blocked coronary artery, valvular heart disease, or congenital cardiac defect.
• In some patients, there may be a need for implantable cardio-converter defibrillator (ICD).
3. Stage C
Patients that are having Stage C heart failure have previously been diagnosed with HF and may have or had signs and symptoms of heart failure. This is a more advanced stage with the following symptoms:
• Fatigue (because of inadequate oxygen supply to tissues)
• Breathlessness
• Lethargy
• Edema (swelling because of fluid retention)
Treatment options
Same treatment as suggested for stage A and B
- Treatment of other comorbidities e.g hypertension, diabetes mellitus
- Aldosterone antagonist (to prevent fluid retention) as aldosterone acts in a way to increase blood volume.
Ivabradine is additionally added for symptomatically treating heart-related chest pain
4. Stage D
Stage D of heart failure is associated with the symptoms that can’t be treated with medication or supportive therapy. The patient is needed to hospitalize recurrently despite all treatment measures. This is the end-stage of heart failure.
Treatment options
General treatment for patients with Stage D involves:
• Treatments options of Stages A, B, and C.
• Choosing more advanced treatment, for example:
- Cardiac transplantation
- Ionotropic drugs via the intravenous route
- Cardiac surgery
Summary
There are four stages of heart failure, stage A, B, C, and D. Heart failure gradually worsens and stage D is the end stage of heart failure with no effect of therapy.
What are the properties of cardiac physiology and pathophysiology?
There are following functional properties of the heart that if disturbed, lead to heart failure:
1. Preload
Preload is the stretching of cardiac muscles at the end of the diastole. Pressure in left atria is a determining factor of preload. The more the preload more is the blood in the heart.
Pathophysiology:
Preload is generally increased in heart failure because of increased blood volume and venous pressure
. ### 2. Afterload:
Afterload is the resistance against which the heart has to contract for the ejection of blood. If there is resistance in vessels that will receive the blood, the heart has to contract more forcefully.
Pathophysiology:
Afterload is increased as a result of increased vascular resistance and aortic pressure. When afterload increases, stroke volume decreases.
3. Contractility
The strength and force with which the heart contracts in the systolic phase is called contractility.
As contractility decreases in the heart, there is a reduction in the velocity of muscle shortening.
When contractility is increased by an increased influx of calcium, the heart has to work with more vigor, which is dangerous for the weakened heart.
4. Heart rate
Heart rate is the speed with which the heartbeats. It is calculated by the number of beats per minute. Heart rate is a major factor to determine cardiac output.
Cardiac output is the product of heart rate and stroke volume.
Hence decreased heart rate results in decreased cardiac output and decreased supply of blood to body tissues.
As heart rate decreases in failure and stroke volume are reduced, the sympathetic system acts to increase the heart rate and hence act as a compensatory mechanism.
Summary
Preload, afterload, contractility, and heart rate are the physiological parameters. If these parameters deviate from the normal pattern, it may lead to heart failure.
What is the treatment of heart failure?
There are seven classes of drugs that are effective in the treatment of heart failure.
1. Angiotensin-converting enzyme inhibitors (ACEIs)
They include Captopril, enalapril, lisinopril, etc.
Mode of action:
Angiotensin is a hormone that acts as a vasoconstrictive agent. Vasoconstriction can increase the workload on the heart, by increasing preload and afterload. ACEIs suppress the formation of that hormone and hence act as vasodilators. They decrease preload and afterload and compensate for the heart.
2. Angiotensin-receptor blockers
They include losartan, valsartan, telmisartan etc.
Mode of action:
Their actions result in the same effects as ACEIs except for the mechanism of suppressing angiotensin hormone levels. They block the receptor at which angiotensin acts and hence cause vasodilation.
3. Aldosterone antagonists
They include spironolactone, eplerenone. Aldosterone antagonists are diuretics and also known as water pills.
Mode of action
They act to reduce blood volume hence decreasing blood pressure and compensating weakened heart.
4. β-blockers
Beta-adrenergic blocking agents include propranolol, carvedilol, timolol, atenolol**, etc.
Mode of action:
Beta-blockers block the beta receptors in the heart. A blockade of these receptors inhibits the effect of epinephrine (a sympathetic neurotransmitter) and hence decreases blood pressure and heart rate.
5. Diuretics
Also known as water pills. They excrete excessive water from the body through the kidneys and hence decrease the blood volume and hence blood pressure and swelling of feet, ankles, etc. Important examples of diuretics are furosemide, bumetanide, and hydrochlorothiazide.
6. Vasodilators
They cause the dilation of veins leading to a decrease in cardiac preload by increasing capacitance of veins. The most important vasodilators are Nitrates.
7. Ionotropic agents
These are the drugs that increase the contractility of the heart by increasing the intracellular calcium level and hence increase the cardiac output.
1. Digitalis glycosides
- Also known as cardiac glycosides and mostly obtained from the digitalis plant. Digitalis glycosides are chemically similar compounds that enhance the contraction of cardiac muscle and hence are used in the treatment of heart failure.
- One of the important properties of digitalis glycosides is that they are associated with low therapeutic index i.e. there is a very small difference between a therapeutic dose and a toxic dose. The most frequently used cardiac glycoside is Digoxin.
2. β-Adrenergic agonists
β-receptors agonists, for example dopamine and dobutamine also act to improve the function of the heart by increasing contractility and vasodilatory effects. After Digoxin, the second most common agent is dobutamine.
3. Phosphodiesterase inhibitors
PDEIs such as Milrinone increase contractility of the heart by increasing intracellular levels of cyclic adenosine monophosphate (cAMP) leading to an increased influx of calcium.
Summary
In the treatment of heart failure, mainly used therapy includes ACEIs, ARBs, aldosterone antagonists, beta receptors blocking agents, certain diuretics, vasodilating agents, ionotropic agents, beta adrenergic agonists and phosphodiesterase inhibitors.
Frequently Asked Questions
1. How long can you live with heart failure?
The expected life span for the patients with heart disease is variable according to the level of disease. Some other factors like the age of the patient, genetic profile, and other comorbidities also determine how many years a heart patient can live .According to the research of the Centre for Disease Control (CDC), half of the patients with heart failure can live more than five years if they are adherent to medication and preventive measures.2. What is the main cause of heart failure?
In most cases, several other diseases, including diabetes, arteriosclerosis, myocardial infarction, obesity, hypertension, and coronary artery defects can be a major cause of heart failure.
Family history of cardiomyopathy and congenital heart disease can also be a reason for heart failure.
3. Can depression cause a heart attack?
In the individuals that are already suffering from cardiac disease, depression can exacerbate the condition. While in the people with no previous heart problem, depression anxiety and stress can enhance the chances of developing heart disease and heart attack.
4. Is low blood pressure a symptom of heart failure?
Moderately low or extremely low blood pressure indicates that the myocardial muscles have become so weakened that the heart is unable to contract properly and pumping of blood is difficult resulting in low cardiac output. Low blood pressure and syncope is a sign of heart disease and maybe heart failure.
5. What are the signs of worsening heart failure?
The following signs and symptoms indicate the worsening heart failure:
- Rapid and unexpected increase in body weight
- Oedema in certain body parts i.e. feet and ankles.
- Abdominal pain
- Nocturnal breathlessness
- Difficulty to walk or climb the stairs
- Shortness of breath at rest, with no physical activity
- Fatigue and loss of appetite
- Wheezing and disorientation
Conclusion
Heart failure is a chronic, progressive disorder of the heart that occurs due to some underlying cause, for example, myocardial infarction, cardiomyopathy, hypertension, or ischemic heart disease, etc. Normal physiological parameters including preload, afterload, contractility, and cardiac output if getting disturbed, can cause heart failure. Beta-blockers, vasodilators, ACEIs, ARBs, Aldosterone antagonists, inotropic agents and diuretics are the preferred treatment for heart failure.