Headache is a very common problem that most people will experience many times during their lives. It is a pain in the head or face. This pain can be throbbing, constant, sharp or dull. Headache can be treated with medication, stress management and biofeedback.

Why headaches are common in adults?
If the head is throbbing, it doesn’t mean that you are alone. Headache is one of the most common pain conditions in the world. Headaches may be the cause of hypertension and stress. Up to 76% of youths worldwide have had a headache in the past year.
It is considered as a major cause of absenteeism from work and school. They also take a toll on social and family life. Some people thinks that, continually battling headaches can lead to feeling anxious and depressed.
Headaches in children
Most children have had a headache by the time they get to high school. For about 21% of them, tension headaches and migraines are a reoccurring problem. Similar to adults, triggers for headaches in children include:
- Environmental factors.
- Certain foods that trigger headaches for the individual.
- Changes in sleep.
- Stress.
![]()
What are the types of headaches?
There are almost more than 150 types of headache. They types of headache fall into two main categories: primary and secondary headaches.
1. Primary headaches
Primary headaches aren’t due to another medical condition. Primary headache includes:
-
Cluster headaches:
Cluster headaches occur in cyclical patterns or cluster periods. These are one of the most painful types of headache. A cluster headache is most commonly awakens in the middle of the night with intense pain in or around one eye on one side of the head.
Bouts of frequent attacks, known as cluster periods. It can last from weeks to months. It usually followed by remission periods when the headaches stop. During remission there is no headaches occur for months and sometimes even years.
Fortunately, this type of headache is rare and not life-threatening. Through treatments, it is possible to make cluster headache attacks shorter and less severe. In addition, medications can reduce the number of cluster headaches.
Symptoms
Common sign and symptoms of cluster headaches
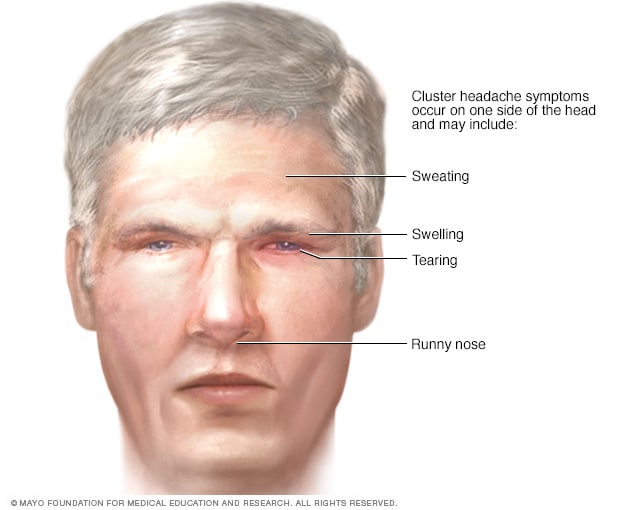
A cluster headache strikes quickly, usually without warning, although a person might first have migraine-like nausea and aura. Common signs and symptoms during a cluster headache include:
- It is one-sided pain
- Excruciating pain that is normally situated in, behind or around one eye, but may transfer to other areas of face, head and neck
- Drooping eyelid on the affected side
- Skin paling or flushing on face
- Excessive tearing
- Redness of the eye on the affected side
- Stuffy or runny nose on the side of pain
- Forehead or facial sweating.
- Restlessness
- Swelling around eye on the affected side
Causes
The exact cause of this type headaches is unknown. Cluster headache patterns suggest that abnormalities in the body’s biological clock (hypothalamus) play a role.
Cluster headache generally isn’t associated with triggers, such as foods, hormonal changes or stress.
Once this period begins, however, drinking alcohol may trigger a splitting headache. For this reason, many people with cluster headache avoid alcohol during a cluster period.
Other possible triggers for the headache include the use of medications such as nitroglycerin, a drug used to treat heart disease.
Risk Factors for Cluster Headaches
Risk factors for cluster headaches include:
Sex. Men have more chances to have cluster headaches.
Age. Most of the people who develop cluster headaches are between ages 20 and 50, although the condition can develop at any age.
Alcohol use. If you have cluster headaches, drinking alcohol during a cluster period may increase your risk of an attack.
Smoking. Smokers have mostly attacked of cluster headaches. However, quitting smoking usually has no effect on the headaches.
A family history. Having a parent or sibling who has had cluster headache might increase your risk.
When to see a doctor?
See the doctor if you’ve just started to have cluster headaches to rule out other disorders and to find the most effective treatment.
Headache pain, even when severe, usually isn’t the result of an underlying disease. But headaches can occasionally indicate a serious underlying medical condition, such as a brain tumor or rupture of a weakened blood vessel (aneurysm).
If you have a history of headaches, see the doctor if the pattern changes or headaches suddenly feel different.
Diagnosis
This type of headache has a characteristic type of pain and pattern of attacks. A diagnosis of cluster headache depends on the description of the attacks, including pain, the location and severity of the headaches, and associated symptoms.
Neurological Examination
A neurological examination can help the doctor to detect physical signs of a neurological disorder. The exam is usually normal in patients with cluster headaches. The doctor will use a series of procedures to analyze your brain function, including testing your senses, reflexes and nerves.
Imaging Tests for Cluster Headaches
If a person has unusual or complicated headaches or an abnormal neurological examination, the doctor might recommend other tests to rule out other serious causes of head pain, such as a tumor or an aneurysm. Common brain imaging tests include:
- MRI. This uses a powerful magnetic field and radio waves to produce detailed images of the brain and blood vessels.
- CT scan. This uses a series of X-rays to create detailed cross-sectional images of the brain.
Treatment
There is no proper cure for cluster headaches. The goal of treatment is to decrease the severity of pain, shorten the headache period and prevent the attacks.
Because the pain of a cluster headache comes on suddenly and might subside within a short time, cluster headache can be difficult to evaluate and treat, as it requires fast-acting medications.
Some types of acute medication can provide some pain relief quickly.
- Migraine.
Migraine is a neurological condition of a person that can cause multiple symptoms. It is frequently characterized by intense, debilitating headaches.
Migraines may begin in childhood or may not occur until early adulthood. Women are more likely than men to have migraines. Family history is one of the most common risk factors for having migraines.

Symptoms of Migraine
Symptoms of migraine may begin one to two days before the headache itself. This is known as the prodrome stage. Symptoms during this stage may include:
- food cravings
- neck stiffness
- depression
- hyperactivity
- fatigue or low energy
- frequent yawning
- irritability
The aura occurs after the prodrome stage. During an aura, a person may have problems with vision, sensation, movement, and speech. Examples of these problems include:
- seeing shapes, light flashes, or bright spots
- difficulty speaking clearly
- temporarily losing vision
- feeling a prickling or tingling sensation in face, arms, or legs
The next phase this type of headache is known as the attack phase. This is the most acute or severe of the phases when the actual migraine pain occurs. In some people, this can overlap or occur during an aura. Attack phase symptoms can last anywhere from hours to days. Symptoms of a migraine can vary from person to person. Some symptoms may include:
- dizziness or feeling faint
- increased sensitivity to light and sound
- nausea
- vomiting
- pain on one side of head, either on the left side, right side, front, or back, or in temples
- pulsing and throbbing head pain
What are the causes of migraines?
The causes of migraines have not yet identified. However, researchers have found some contributing factors that can trigger the condition. This includes changes in brain chemicals, such as a decrease in levels of the brain chemical serotonin.
Factors that may trigger a migraine include:
- changes in barometric pressure
- bright lights
- severe heat, or other extremes in weather
- dehydration
- hormonal changes in women, such as estrogen and progesterone fluctuations during ■■■■■■■■■■■■, pregnancy, or menopause.
- excess stress
- loud sounds
- skipping meals
- changes in sleep patterns
- smoking
- alcohol use
- traveling
Treatment
The people who have migraines find that over-the-counter painkillers, such as paracetamol, aspirin and ibuprofen, can help to reduce their symptoms. They tend to be most effective if taken at the first signs of a migraine attack, as this gives them time to absorb into their bloodstream and ease symptoms.
- New daily persistent headaches (NDPH).
New daily persistent headache (NDPH) begins suddenly then occurs every day over a long time. The defining feature of this type of headache is that you clearly remember the circumstances, sometimes even the exact date, of the first headache.
Characteristics of NDPH
- It’s not caused by another underlying condition
- This headache becomes persistent, occurring every day, within 24 hours of onset.
- The headache is continuous for three months or more.
- The onset is clearly remembered and can be pinpointed.
- The headache is not previous chronic headaches occurring more often.

Symptoms of NDPH
Symptoms of NDPH is common to all cases of NDPH are remembering its onset, which is sudden, and having persistent daily headache.
Symptoms of NDPH involve headache pain that:
- is usually moderate to severe
- sometimes has migraine-like associated symptoms of nausea and vomiting or sensitivity to light, called photophobia.
- is usually either throbbing like a migraine or tightening like a tension headache
- is usually on both sides of the head but can be only on only one side
- may get better or worse over the day
What are the causes of NDPH?
Chronic daily headaches are either primary with an unknown cause, or secondary where the cause is another underlying condition. NDPH is always a primary condition. If a secondary cause is found, the diagnosis is the underlying condition. These include:
- temporal arteritis
- bleeding around the brain, such as with a subdermal hematoma or epidural hematoma
- pseudotumor cerebri, increased spinal fluid pressure
- blood clot in the veins of the brain
- head injury
- medication overuse
- meningitis
- spinal headache
Is there a treatment for NDPH?
There are two subtypes of NDPH:
Very few researches have been done on the treatment of NDPH, and no medication has been proven to be effective. Initial treatment is usually based on the type of headache the symptoms resemble the most: migraine or tension. The doctor may give different medications to try to find out what works best.
Medications that might be used include:
-
tricyclic antidepressants, such as amitriptyline or nortriptyline
-
antiseizure medication, such as gabapentin(Neurontin) or topiramate
-
triptans typically used for migraine, such as almotriptan (Axert) or sumat riptan
-
selective serotonin reuptake inhibitors (SSRIs)such as fluoxetine or sertraline
-
muscle relaxants, such as baclofenor tizanidine
-
nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofennaproxen
-
Tension headaches.
A tension headache is generally a diffuse, mild to moderate pain in the head that is often described as feeling like a tight band around the head. A tension headache is the most common type of headache.
Symptoms of Tension Headache
Signs and symptoms of a tension headache are:
- Tenderness on scalp, neck and shoulder muscles
- Sensation of tightness or pressure across forehead or on the sides and back of the head
- Dull, aching head pain
Tension headaches are mainly divided into two categories:
Episodic tension headaches
Episodic tension headaches can last from 30 minutes to a week. Frequent episodic tension headaches occur less than 15 days a month for at least three months. Frequent episodic tension headaches may become chronic.
Chronic tension headaches
Chronic tension headache lasts hours and may be continuous. If headaches occur 15 or more days a month for at least three months, they’re considered chronic.
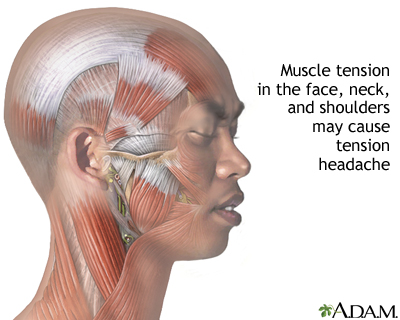
Causes of Tension Headaches
The cause of tension headaches is not known yet. researchers used to think tension headaches stemmed from muscle contractions in the face, neck and scalp, perhaps as a result of heightened emotions, tension or stress. But recent researches suggest muscle contraction isn’t the cause.
The most common research supports a heightened sensitivity to pain in people who have tension headaches. Increased muscle tenderness, a common symptom of tension headaches, may result from a sensitized pain system.
Preventive Measures
In addition to regular exercise, techniques such as biofeedback training and relaxation therapy can help reduce tension headache.
- Biofeedback training. This technique teaches to control certain body responses that help reduce pain. During a biofeedback session, people are connected to devices that monitor and give feedback on body functions such as muscle tension, heart rate and blood pressure. people then learn how to reduce muscle tension and slow your heart rate and breathing themselves.
- Cognitive behavioral therapy. This type of talk therapy may help people learn to manage stress and may help reduce the frequency and severity of their headaches.
- Other relaxation techniques. Anything that helps relax, including deep breathing, yoga, meditation and progressive muscle relaxation, may help headaches. people can learn relaxation techniques in classes or at home using books or tapes.
Medications
Using medications in stress management techniques may be more effective than is either treatment alone in reducing tension headaches.
Additionally, living a healthy lifestyle may help prevent tension headaches:
- Don’t smoke.
- Eat regular, balanced meals.
- Get enough, but not too much, sleep.
- Exercise regularly.
- Limit alcohol, caffeine and sugar.
2. Secondary headaches
Secondary headaches are headaches that are due to an underlying medical condition, such as a neck injury or a sinus infection. Secondary headache may be a sign of a serious underlying medical condition such as: brain infection such as encephalitis or an abscess. brain tumor.
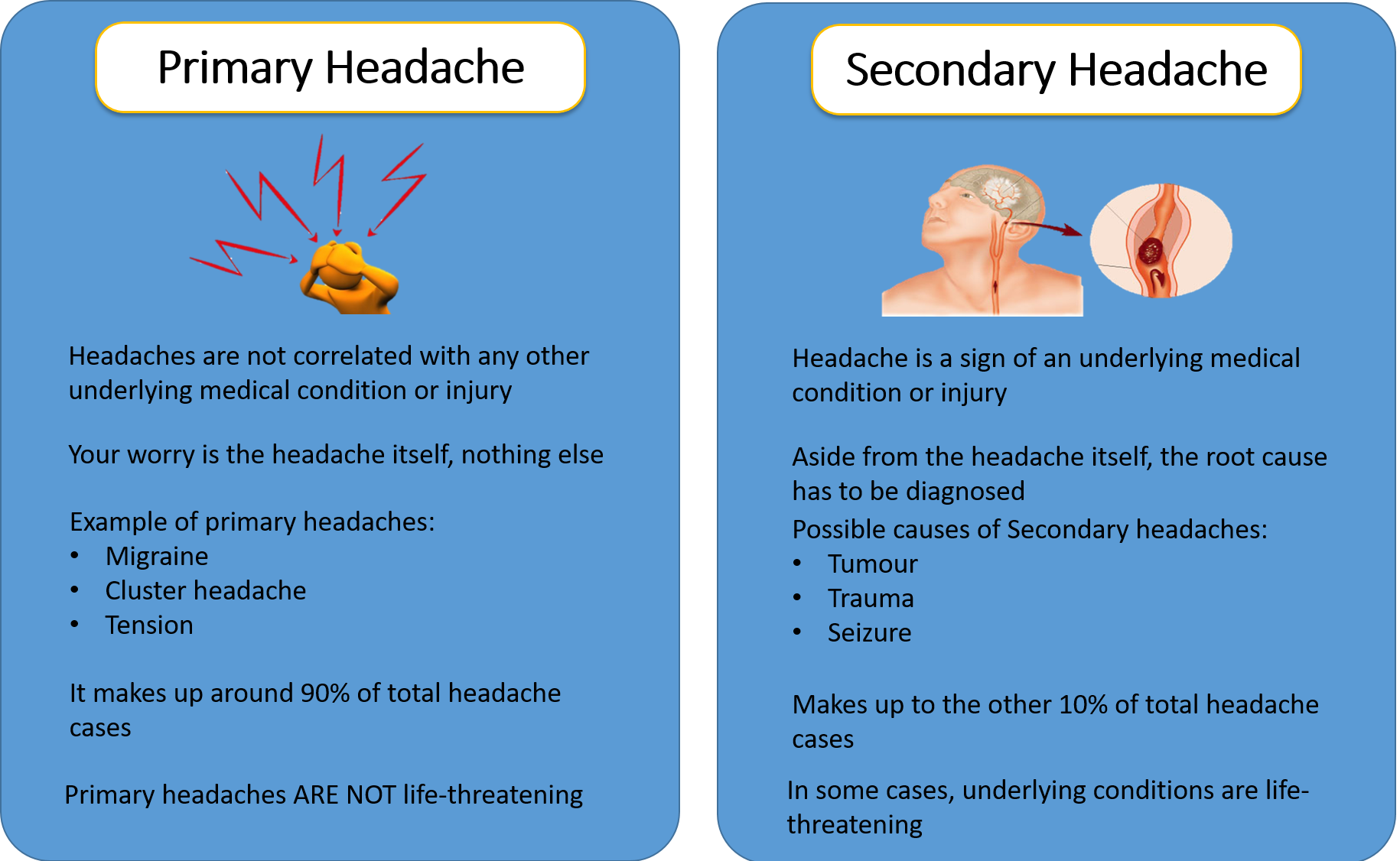
Secondary headaches are related to another medical condition, including:
- Medication overuse.
- Disease of blood vessels in the brain.
- High blood pressure (hypertension)
- Head injury.
- Sinus congestion.
- Infection.
- Tumor.
- Trauma.
Natural Remedies to Get Rid of Headache
There are many natural methods that people can try to help them get rid of a headache. These remedies are:
- Water

Drinking enough water may help prevent headaches or reduce their severity and stop dehydration which can be an underlaying cause of headache.
Slight dehydration may alter how people think and function, making them feel worse, with or without a headache.
Water may help make someone in this situation feel better, although some studies are more cautious.
- Cold Compress
A cold compress can be a simple headache solution that many people have on hand. Applying an ice pack or another cold item to the head or neck may help constrict the blood vessels and reduce inflammation in the area. Doing so could temporarily relieve headache pain.
- Warm Compress
In tension headache where the muscles are too tight, a warm compress may help relax these muscles and bring relief.
A warm compress might be as simple as a heated towel. People may be able to get the same effect from a tepid shower or bath.
- Turn Down the Lights
Some people who get headaches become sensitive to light. Bright office lights or even the bright light from a smartphone may make symptoms worse.
It may help to rest in a dark or dimly lit room to recover from a headache.
- Exercise
Exercise can help keep the body healthy and promote better circulation, which could reduce the chances of a headache showing up.
Frequently Asked Questions
Here are frequently asked questions related to the topic how to get rid of headaches.
- What gets rid of a headache fast?
Try the following tips and get to feeling better fast
- Ease pressure on your scalp or head.
- Try a cold pack. If you have a migraine, place a cold pack on your forehead.
- Use a heating pad or hot compress.
- Try not to chew.
- Dim the lights.
- Practice relaxation.
- Get some caffeine.
- Take some ginger
- What causes headaches everyday?
Conditions that may cause nonprimary chronic daily headaches including Inflammation or other problems with the blood vessels in and around the brain, including stroke. Infections, such as meningitis. Intracranial pressure that’s either too high or too low.
- What does a blood pressure headache feel like?
Researchers are still unsure if high blood pressure causes headaches. According to a recent research, headaches are due to high blood pressure typically occur on both sides of the head. The headache pain tends to pulsate and often gets worse with physical activity.
- Why won’t my headache go away?
If the problem in your neck isn’t treated, your headache won’t go away. Cervicogenic headaches be caused by injuries, arthritis, bone fractures, tumors, or infection. Your body posture or falling asleep in an awkward position could cause a cervicogenic headache.
-
What should I eat for headache?
-
dried or cooked fruits, particularly non-citrus kinds such as cherries and cranberries.
-
orange, yellow, and green vegetables, such as summer squash, sweet potatoes, carrots, and spinach.
-
rice, especially brown rice.
-
carbonated, spring, or tap water.
Conclusion:
Migraine is a disorder associated with significant psychosocial impact. The diagnosis of migraine requires a good clinical history, and exclusion of other causes of headache. However, further investigations are needed when the findings from the history and clinical examination are atypical of migraine, or if there is a recent change in the character of the patient’s headaches.
Current pharmaceutical anti-migraine treatments have revolutionized migraine management. Optimal treatment needs to be individualized, taking into consideration side effects of medications, duration and severity of symptoms, and outcome of previous treatments.
Must read these topics